Red Light, Blue Light
Using the correct LED wavelength to improve the skin, Part 1
This article originally appeared in the February 2020 issue of Dermascope Magazine.
The increasing demand by the client seeking noninvasive procedures for improving medical and aesthetic dermatologic conditions has led to the increased demand for light emitting diode (LED) therapy in aesthetic practices.
Research on LED mechanisms of action has shown to have multiple pathways in which there is quantifiable clinical benefits. The use of wavelengths has measurable benefits to both the client and the professional in terms of outcome with no side effects or complications.
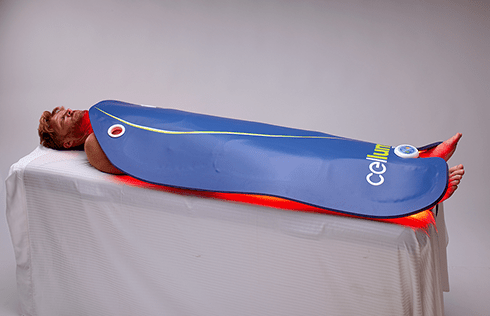
Modern LED devices are able to target large areas depending on the clinical conditions being treated thereby reducing treatment time and improving outcomes.
There are numerous dermatological and medical conditions that benefit from the use of LED therapy. A 2018 study reviewed randomized controlled trials in medical and dermatological conditions. Their findings support the significant benefits in the use of LED for acne, herpes zoster, skin rejuvenation, and psoriasis.
Medical conditions such as acute and chronic wound healing, management of pain, and inflammatory joints have all shown to be clinically benefited by LED. In cases of radiation dermatitis, oral mucositosis, and atopic dermatitis, further studies are required to demonstrate a statistical benefit.
Beneficial Wavelengths
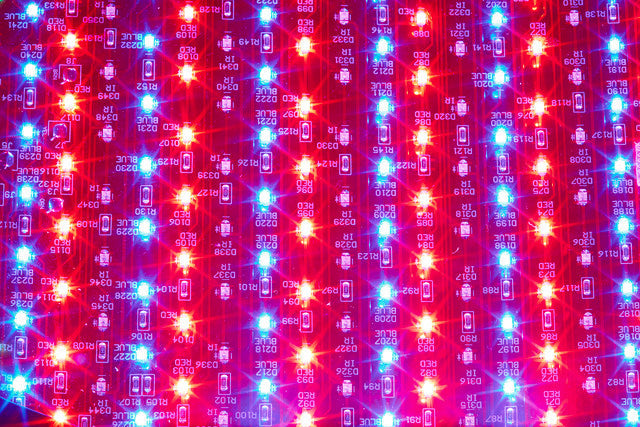
The depth of each wavelength adopted in LED therapy — blue, red, and near infrared — have differing primary targets and photoreactions in the target cells through photon absorption, intracellular signal transduction, and the cellular photo response.
Visible wavelengths stimulate cellular metabolism by triggering intracellular photobiochemical reactions. The observed effects include increased adenosine triphosphate — an organic chemical that provides energy — modulation of reactive oxidative species, alternation of collagen synthesis, stimulation of angiogenesis, and increased blood flow.
Studies have also demonstrated the increase in the production of multiple growth factors and the inhibition of apoptosis or cellular death. All studies have demonstrated a statistically significant improvement in skin rejuvenation, as well as enhancing existing rejuvenation treatments.
Clinical studies in the use of red LED (630 to 700 nanometers) have demonstrated it activates fibroblast growth factors, increasing type 1 procollagen, an increase in matrix metalloproteinase-9 (MMP-9), and a decrease in MMP-1.
These result in the reduction of fine lines and wrinkles, improvement in photo-aging, a decrease in melanin, and softer, smoother, healthier looking skin. Skin analysis studies reveal an increased collagen density in the papillary and upper reticular dermis with the collagen bundles more packed and well organized. The thickness was observed to be greater than when evaluated before red LED treatment.
Red LED has also proven to extend the remission intervals in those with recurrent herpes simplex infections from 30 to 73 days. The mechanism of action is unclear but it is suggested that there is a delayed inhibitory effect of LED on hypersensitivity reactions.
Yellow light penetrates a depth of 0.5-2 millimeters (570 to 590 nanometers) and has been shown to have benefit in treating skin conditions involving redness, swelling, and photo-aging.
However, due to its shallow reach, there is little evidence to support its use as a single modality, as the above mentioned benefits are better achieved with the application of red light, which carries additional stimulatory and anti-inflammatory benefits and, more importantly, the red wavelength is capable of reaching deeper into the dermal layer and, therefore, reaching more of the target cells.
The same argument applies to green wavelengths, which are simply too short to reach the target cells located in the dermis.
The management of inflammatory and autoimmune skin conditions, such as acne vulgaris, rosacea, and psoriasis, have shown dramatically significant improvement with LED therapy.
In cases of acne, there is a multifactorial influence in the proliferation of acne: thickening of the epithelial layers in the follicles, increased sebum production due to androgenic hormone secretions, colonization of P.acnes bacteria, and inflammation.
The bacterium plays a key role in the release of cytokines that, in turn, triggers the inflammatory reactions and alters keratinization. The use of topical and oral treatments currently available in the management of this debilitating condition can either be ineffective or poorly tolerated by the clients.
This results in poor outcomes and a resurgence of the condition that has a social and psychological impact on those affected by acne.
The use of blue light (400 to 470 nanometers) is most suitable for superficial conditions. Its depth of penetration is limited to less than 1 millimeter and a single modality has been clinically proven to be significantly effective in managing acne vulgaris.
The mechanism of action responsible is the absorption of the light by porphyrins produced by the bacteria, which sets off a photochemical reaction and forms reactive free radicals and singlet oxygen species, which in turn leads to bacterial destruction.
This appears to be highly effective in the management of non-inflammatory acne. Given that acne is a multifactorial skin condition, treatments need to be able to target all four influences. Blue light emits an anti-inflammatory effect that appears to be a result of a shift in cytokine production. Red light stimulates the increase in collagen production, supporting wound healing necessary for resolution and a reduction in scarring.
The combination of red and blue light has been demonstrated to have a significant inhibitory effect on sebum production, as well as the reduction in the inflammatory processes associated with acne vulgaris. Red light has been proven to reduce sebum proliferation.
Various studies have conclusively demonstrated a significant improvement in the use of combined red and blue light used twice weekly for six to eight weeks compared to the use of topical benzyl peroxide.
A similar study comparing topical antibiotic with blue light found an overall reduction by 34% in inflammatory acne with blue light, compared to 14% for the topical antibiotic. Adopting both blue and red wavelengths in the management and treatment of inflammatory acne dramatically improves outcomes, psychological well-being, and quality of life.
More recent studies have shown promise in the benefits for those suffering from psoriasis and rosacea. Both conditions are autoimmune, inflammatory disorders with clinical symptoms of redness, flushing, and dryness. Evidence is scarce, yet there is supportive evidence to suggest that a combination of blue and red light helps to reduce the inflammatory process in psoriasis and rosacea.
Some suggest the combination of red and near-infrared offers improvement. Evidence supports the amelioration of symptoms of both diseases, but in the case of psoriasis, there is the potential of the return of symptoms on cessation of treatment. It is incumbent that the professional manages expectations when managing complex autoimmune skin conditions, with the focus on improvement rather than resolution.
The management of deeper wounds, burns, ulcers, and lesions has proven to benefit from the use of the invisible wavelength, near-infrared light (800 to 1200 nanometers), the deepest penetrating wavelength. Numerous studies, however, suggest the combination of near-infrared and red light dramatically accelerates wound healing, reduces pain and erythema in tissue trauma, and chronic ulceration.
There are also benefits in the use of near-infrared in post-surgery recovery to accelerate wound healing and reduce the risk of the development of keloids and hypertrophic scars. This is as a result of increased collagen and elastin synthesis and the stimulation of interleukin IL6, platelet derived growth factors (PDGF), and transforming growth factors (TGF) that has a direct impact on the increase of hyaluronic acid demand by the fibroblasts and subsequent increase collagen synthesis.